
Once a shoulder joint becomes dislocated, it’s more likely to become unstable.
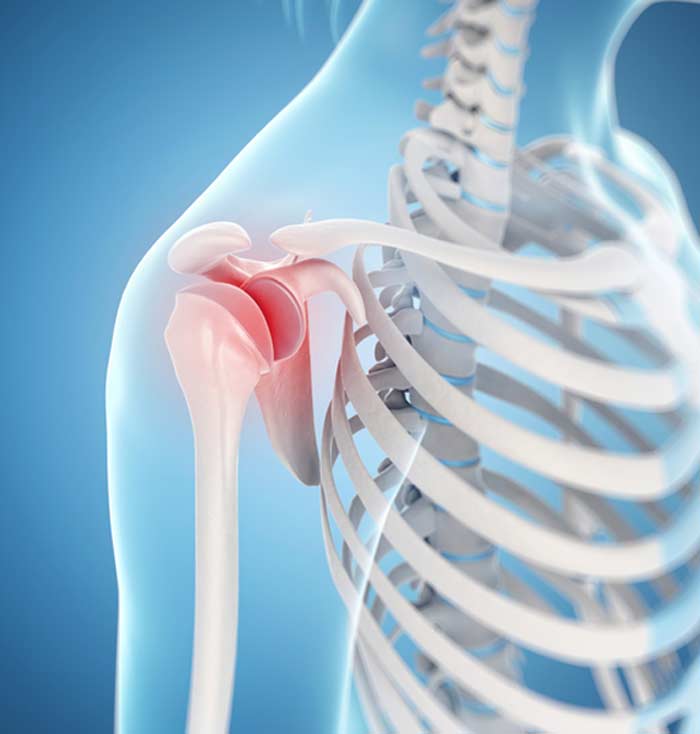
If the ball part of the shoulder’s ball-and-socket (humeral head) regularly moves partially or completely out of its proper position in the socket, it’s a condition referred to as shoulder instability.
The shoulder joint is especially susceptible to instability because it’s the most movable joint in the human body, which increases the risk of strain from overuse or over-extension or injury.
What Causes or Contributes to Shoulder Instability?
The most common way for a shoulder to become unstable is for some type of trauma or injury to occur, such as a hard impact while playing sports or falling, which causes the shoulder joint to dislocate. If the humeral head is partially or completed dislocated, nearby ligaments and the cartilage rim around the shallow “socket” (glenoid) may become damaged or torn.
It’s also possible to develop instability without dislocating the affected shoulder. This may happen from repetitive strain caused by activities such as tennis and swimming that require constant shoulder motion and stress. People who naturally have looser shoulder ligaments are also at a greater risk for developing instability. In rare instances, a shoulder may become unstable without a history of dislocation or repetitive stress injuries.

What Are Signs and Symptoms of an Unstable Shoulder?
Some people feel the ball part of the shoulder dislocate when this joint becomes unstable. This is more likely to happen after a hard fall or impact. The most common sign of an unstable shoulder is sudden or recurring shoulder pain. Additional symptoms experienced may include:
- Recurring instances of the shoulder “giving out”
- Multiple dislocations
- Feeling that the shoulder is unusually loose
- Visible swelling or bruising around the affected shoulder
- Decreased range of motion in the arm and/or shoulder
How Is Shoulder Instability Diagnosed?
During a physical examination, an initial diagnosis of shoulder instability may be made by asking a patient to make certain movements, such as attempting to touch the underside of their forearm with their thumb. Range of motion tests and a check for points of tenderness may also be done. An X-ray is usually taken to rule out other possible sources of instability such as a shoulder fracture and identify a likely reason for the symptoms experienced. MRIs or CT scans are sometimes done if there is a need to view bones and soft tissues in greater detail.
Treatment Options
Unless the instability is severe, initial treatment efforts normally involve temporary immobilization of the affected shoulder with bracing or a sling. Resting for a few days and avoiding certain activities that strain the shoulder may also be recommended. Non-steroidal anti-inflammatory drugs (NSAIDs) are sometimes prescribed to ease swelling. If strengthening shoulder muscles and other types of physical therapy aren’t effective, surgery may become an option. The purpose of surgery is to repair torn or stretched ligaments to increase shoulder stability.
When shoulder instability is corrected with surgery, a sling is usually worn while the joint heals. After the sling is removed, patients begin a rehabilitation process that typically includes range of motion and strengthening exercises. Rehab also reduces the risk of the development of excessive scar tissue and helps ligaments and other soft tissues heal. The duration of recovery will depend the type of surgery performed, patient health, and the extent of participation with physical therapy and rehab efforts.
