Age-related disc wear isn’t reversible, although there are several ways to treat and manage symptoms.
Degenerative disc disease (DDD) is something of a misnomer. It’s not so much a “disease” as it is a general term for the age-related wear can affect any of the 23 discs of the human spine. It’s also a common source of lower back and neck pain, particularly in older adults.
The resulting discomfort can range from minor, low-grade chronic pain that occasionally spikes to severe and debilitating symptoms that may include weakness, numbness, and shooting pain felt in the arms or legs.
Signs, Symptoms, and Commonly Affected Areas
While any spinal disc may be affected by age-related degeneration, it’s often the more mobile and exposed parts of the spine that tend to be affected most. Since the mid-back is protected by the rib cage and internal organs, this means the lower back and cervical spine (neck) are the most common areas affected by DDD. While the level of discomfort associated with degenerative disc disease can vary widely from one individual to the next, the symptoms that are most noticeable and disruptive generally include:
- Lower back pain that extends to the thighs and buttocks
- Neck pain that radiates to the shoulders, arms, or hands
- Discomfort that’s worse when sitting
- Pain that becomes severe when walking or moving
- Pain that’s affected by different positions
- Numbness and tingling sensations in the extremities


Causes and Contributing Factors
If pain is associated with degenerative disc disease, it’s usually because of inflammation or what’s referred to as micro-motions. These so-called micro-motions may contribute to pain if the affected disc’s outer layer (annulus fibrosis) wears down to the point where unnatural motions between vertebrae occur on a consistent basis. These small, abnormal movements may eventually irritate nerve roots, spinal joints, and nearby muscles and other soft tissues. Eventually, an entire spinal segment may become unstable because of these micro-motions. The wear-and-tear of spinal discs can also be affected by poor posture, excess weight, improper lifting techniques, lack of exercise, and poor diet habits.
Diagnosing Degenerative Disc Disease
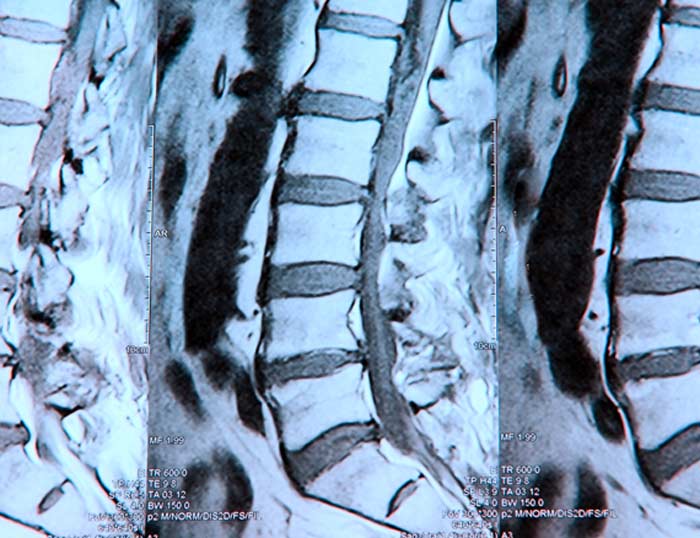
The diagnosis of DDD is based on a physical examination and a review of a patient’s medical history and symptoms. An MRI may be performed to identify disc damage. Nerve conduction studies are sometimes performed to determine if certain nerves are affected. Additional testing may be done to rule out other possible sources of the symptoms being experienced.
Treatment Options for DDD
Unless symptoms are debilitating or potentially life-threatening, treatment for degenerative disc disease typically begins with medication and recommendations to explore various forms of physical therapy. For many patients, a customized exercise plan that includes a focus on core muscle groups helps relieve symptoms by taking some stress off of the spine and its supporting discs. Some patients also benefit from:
- Pain and/or anti-inflammatory medications
- Hot and cold therapy
- Low-impact aerobic activities
- Chiropractic manipulations or adjustments
- Temporary spinal mobilization to allow discs to heal
- Surgery that may include artificial disc replacement or spinal fusion
- TENS units and other forms or mild electrical stimulation
- Lumbar or cervical epidural steroid injections
What’s unique about degenerative disc disease is that symptoms sometimes subside over time as spinal discs naturally settle or move to a location where they aren’t irritating nerve roots. DDD isn’t preventable since age-related changes will eventually affect everyone’s spine. However, eating nutrient-rich foods, staying sufficiently hydrated, remaining within a normal weight range, getting regular exercise, and maintaining good sitting, standing, and sleeping posture may minimize your risk of experiencing disruptive symptoms.
